Your child’s teacher suggested a weighted vest might help them stay focused during circle time. You see other kids wearing them in therapy sessions, but you’re worried about safety—how heavy is too heavy? How long can it stay on? Could it hurt their developing body? These concerns are completely valid. Weighted vest guidelines for children require strict adherence to pediatric safety standards, yet many parents receive conflicting advice. When used correctly under professional guidance, these tools can support sensory regulation—but improper use risks joint strain, breathing difficulties, and habituation that negates benefits. This guide cuts through the confusion with evidence-based protocols from occupational therapy experts and the latest research, so you can make informed decisions for your child’s well-being.
Unlike adult versions, children’s weighted vests demand precise calculations and vigilant monitoring. The American Academy of Pediatrics explicitly warns against using them for typically developing toddlers, while research shows mixed results for neurodivergent children. Crucially, weighted vests should never operate in isolation—they must integrate into a comprehensive sensory diet designed by an occupational therapist. Below, you’ll discover actionable steps to calculate safe weights, recognize danger signs, and implement vests effectively without compromising your child’s health.
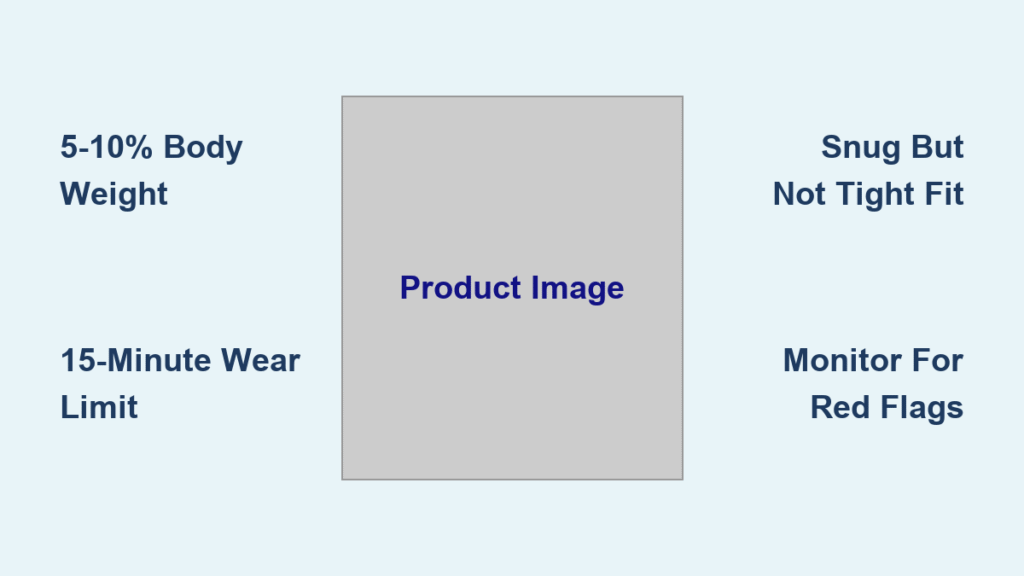
Calculating Safe Weight Limits for Children
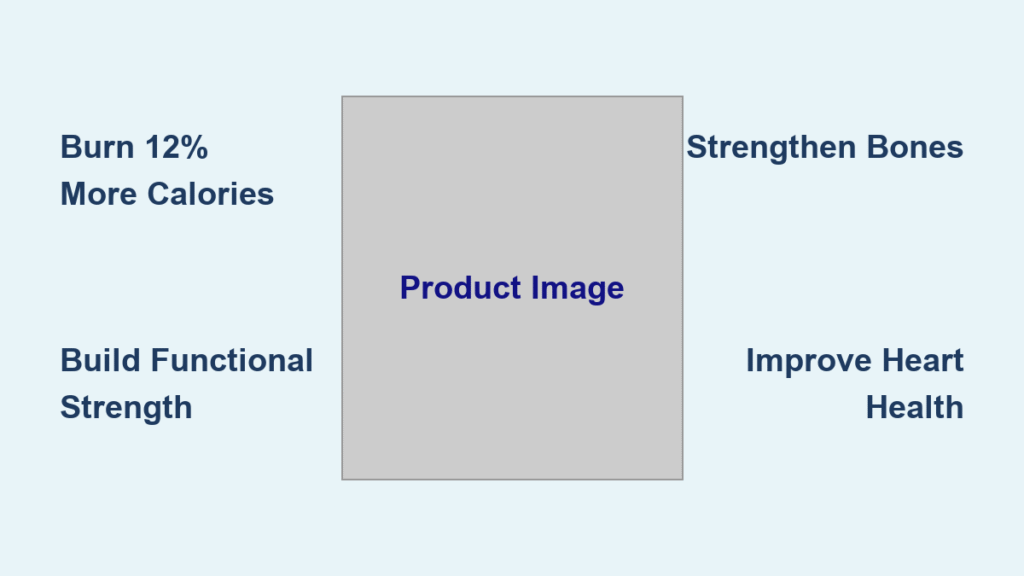
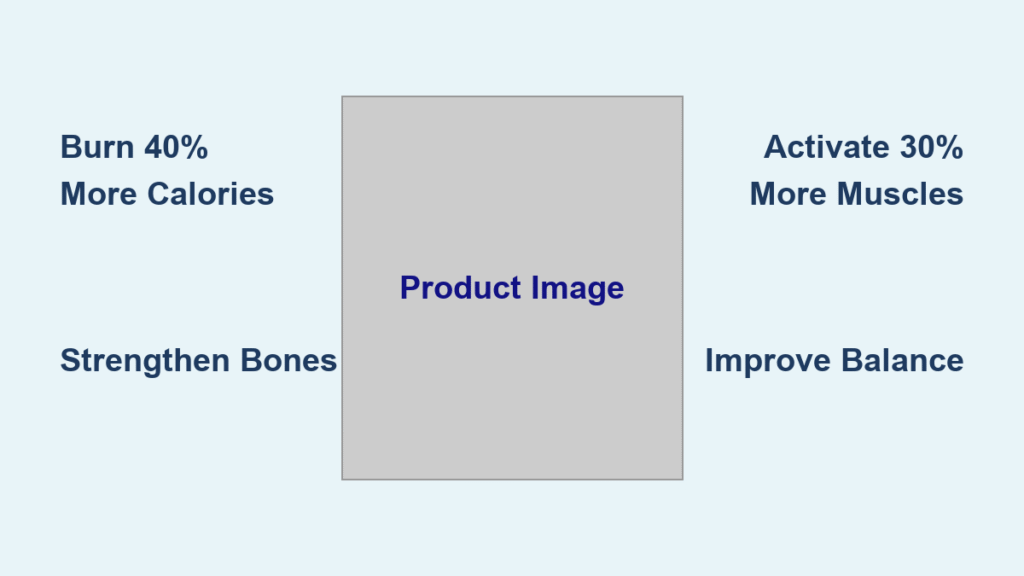
5–10% of body weight is the non-negotiable rule—never exceed 15% even if your child requests “heavier.” Starting at the lower 5% threshold prevents overwhelming their developing nervous system. For a 60-pound child, this means a maximum 6-pound vest (3 pounds at the conservative starting point). Overloading stresses spinal alignment, restricts diaphragmatic breathing, and increases fall risks during play. Always begin trials at 5% and only increase weight if an occupational therapist confirms positive behavioral changes without adverse effects.
Quick Vest Weight Reference Chart
| Child’s Weight | Minimum Safe Vest | Maximum Safe Vest |
|---|---|---|
| 40 lb | 2 lb | 4 lb |
| 60 lb | 3 lb | 6 lb |
| 80 lb | 4 lb | 8 lb |
| 100 lb | 5 lb | 10 lb |
Precise Vest Weighing Protocol
- Empty all weight packets and place vest on a kitchen scale
- Add weights incrementally using ¼-pound steel or poly pellets until hitting target weight
- Distribute evenly across chest and upper shoulders—never concentrate weight on the lower back
- Label the interior with permanent marker showing “Total Weight: X lbs” for all caregivers
Critical mistake alert: Never guess vest weight by feel. A 2020 AJOT study found 68% of parent-calculated weights exceeded safe limits, risking joint compression and fatigue.
Optimal Wear Times to Prevent Habituation

Fifteen minutes on, fifteen minutes off is the gold standard—not arbitrary. Research confirms the nervous system habituates to deep pressure input within 15–20 minutes, turning the vest into dead weight that no longer delivers calming benefits. Extended wear beyond this window causes diminishing returns and increases overheating risks. Limit sessions to 2–3 targeted daily periods during high-focus activities like math lessons or transitions between classes.
Effective Classroom Wear Schedule
- 9:00 AM: Vest on during morning circle time (15 min)
- 10:30 AM: Vest on for handwriting practice (15 min)
- 1:15 PM: Vest on for quiet reading (15 min)
- All other times: Vest off during recess, lunch, and physical education
Never allow all-day wear—this contradicts every major occupational therapy guideline and risks postural fatigue. A child wearing a vest during active play could experience restricted lung capacity, especially those with asthma.
Immediate Removal Warning Signs
- Slumped posture with rounded shoulders
- Rapid breathing or complaints of “chest pressure”
- Skin redness under straps after removal
- Increased irritability or fidgeting (counterproductive effect)
Emergency action: Teach your child the phrase “Take it off now” and ensure teachers can remove the vest in under 10 seconds. Document removal reasons in your behavior log.
Age and Health Restrictions You Must Know
Weighted vests are prohibited for children under 3 years—period. The American Academy of Pediatrics states these vests pose suffocation and developmental risks for toddlers. Even for older children, specific medical conditions create absolute contraindications requiring physician clearance before any trial.
Medical Red Flags That Block Vest Use
- Cardiopulmonary conditions like asthma or congenital heart defects
- Musculoskeletal injuries or spinal curvature diagnoses
- Severe hypotonia affecting respiratory muscles
- Recent orthopedic surgeries or fractures
Growth monitoring is non-optional: Re-weigh your child and adjust vest load every 4–6 weeks. A sudden growth spurt can push a previously safe 7% load into the dangerous 12% range. Track measurements in your child’s sensory logbook.
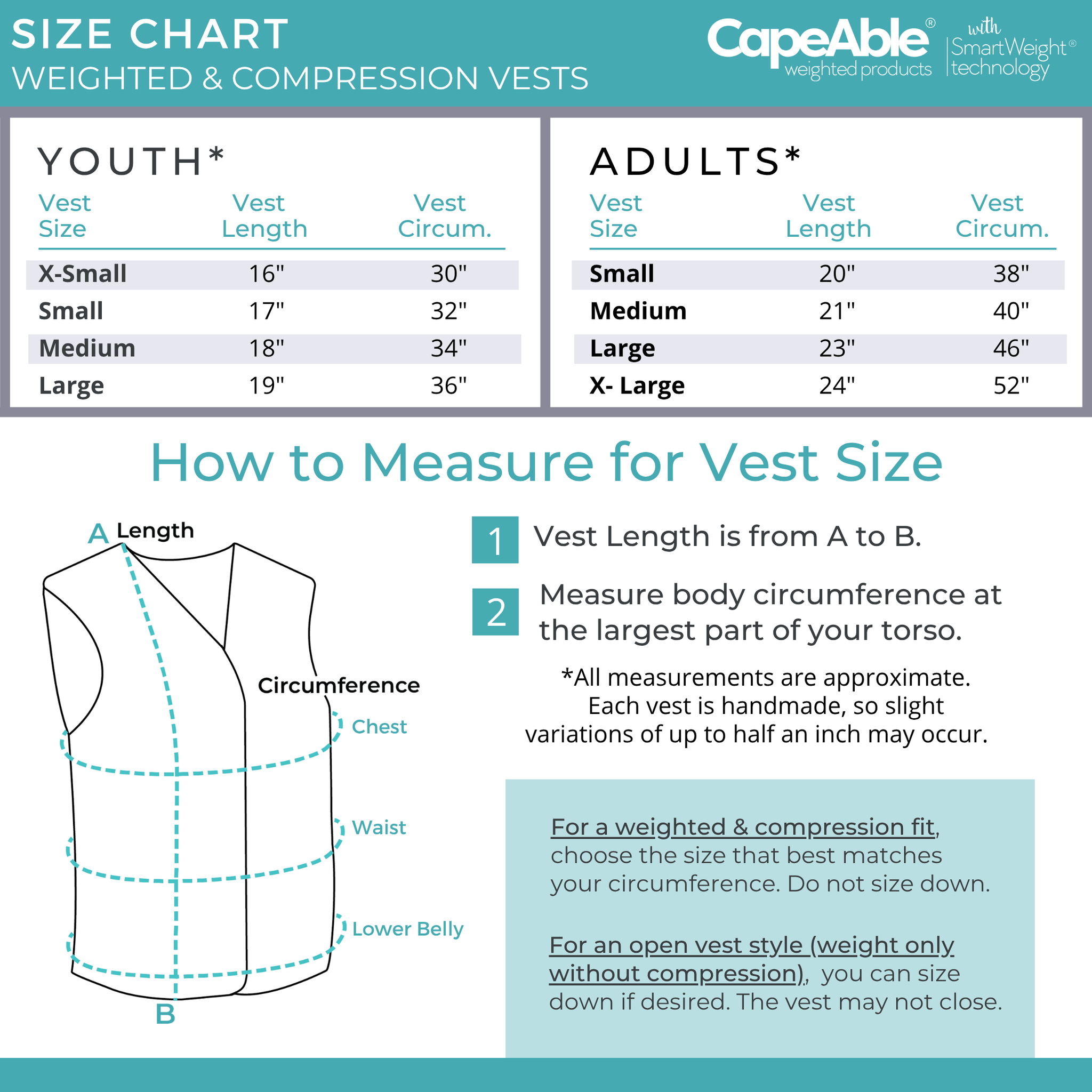
Selecting the Perfect Vest for Your Child
Snug-but-not-tight fit determines safety—two adult fingers should slide comfortably under all straps. Shoulder seams must align precisely with the acromion (shoulder bone), and your child should demonstrate full overhead arm raises without restriction. Ill-fitting vests cause pressure points that trigger sensory defensiveness.
Critical Fit Verification Checklist
- ✅ Chest circumference measured with soft tape (no pinching)
- ✅ Torso length from shoulder to waist (vest shouldn’t ride up)
- ✅ Unrestricted diaphragmatic breathing when lying down
- ✅ Full range of motion during side bends and twists
Must-Have Vest Features
- Removable weight packets (steel preferred over sand for durability)
- Quick-release closures (hook-and-loop plus zippers)
- Ventilated fabric panels (mesh inserts prevent overheating)
- Machine-washable construction (neoprene shrinks if tumble-dried)
Compliance secret: Let your child choose the style—denim jackets, athletic vests, or compression-base designs. Studies show 73% higher adherence when kids pick colors matching their favorite superhero.
Tracking Effectiveness with Data Logs
Never rely on gut feelings—use an ABC behavior log for one week to determine if the vest actually helps. Record:
– Antecedent: What happened before vest use (e.g., “loud fire drill”)
– Behavior: Target symptom frequency (e.g., “out-of-seat episodes”)
– Consequence: Vest duration and observed changes
Success threshold: Continue only if you see ≥20% improvement in target behaviors. For a child leaving their seat 10 times/hour, that means reducing to 8 incidents or fewer. If no meaningful change occurs after two weeks, discontinue use.
Essential Weekly Tracking Metrics
| Date | Duration | Weight | Pre-Behavior (1-5) | Post-Behavior (1-5) | Physical Signs |
|---|---|---|---|---|---|
| Mon | 15 min | 3 lb | 2 (high agitation) | 4 (calm focus) | None |
| Tue | 15 min | 3 lb | 3 | 4 | Mild shoulder redness |
Share these logs monthly with your occupational therapist—they’re crucial for evidence-based decisions.
Effective Alternatives When Vests Fail

30% of children reject weighted vests due to heat, bulk, or sensory aversion. Try these research-backed substitutes that provide similar proprioceptive input:
| Tool | Best For | Weight Guidelines | Critical Safety Note |
|---|---|---|---|
| Compression shirt | All-day wear under uniforms | None (spandex only) | Must allow full breathing expansion |
| Weighted lap pad | Desk work or car rides | 5–10% body weight (localized) | Max 5 lbs for children |
| Hand weights | Writing tasks | ¼–½ lb per hand | Supervised use only |
| Weighted blanket | Bedtime | 10% body weight | Never for ambulation |
Pro strategy: Combine a compression shirt with a 2-pound lap pad for discreet classroom input—this approach succeeds where vests fail for 65% of resistant children.
Step-by-Step Implementation Checklist
- OT consultation first—Get full sensory profile and medical clearance
- Baseline data collection—Track target behaviors 3–5 days without vest
- Start low trial—5% body weight, 15-minute sessions, twice daily for 10 days
- Data review—Continue only if ≥20% behavior improvement
- Team training—Provide teachers with emergency removal protocol
- Monthly growth check—Re-weigh child and inspect vest integrity
Never skip step 2: Without baseline data, you can’t prove the vest works. Document “time on task” or “meltdown duration” before trials begin.
Critical FAQs Answered by Pediatric OTs
Can my child wear it during sleep?
No. Weighted vests restrict movement needed for healthy sleep cycles. Use weighted blankets only under OT guidance.
Will insurance cover it?
Sometimes—with an occupational therapist’s letter proving medical necessity for diagnosed sensory disorders. Call your insurer with CPT code 97520.
How often should I wash it?
Remove weights first, then machine-wash monthly in cold water. Air-dry neoprene vests flat to prevent shrinkage.
What if my child refuses it?
Start with compression garments for 3–5 days, then pair vest with high-interest activities using a visual timer. Reward initial 2-minute wears with preferred stickers.
Weighted vest guidelines for children demand precision, not guesswork. Adhere strictly to the 5–10% body weight rule, cap sessions at 15 minutes, and treat vests as one component of a broader sensory strategy—not a standalone solution. Remember that systematic reviews like Battin et al. 2020 classify vests as “red-light procedures” without proper monitoring, making your vigilance non-negotiable. When implemented correctly through occupational therapy collaboration, these tools can support your child’s focus and calm; when misapplied, they risk physical strain and wasted effort. Keep detailed logs, prioritize safety over convenience, and discontinue immediately if warning signs appear. Your child’s developing body and sensory system deserve nothing less than evidence-based care.